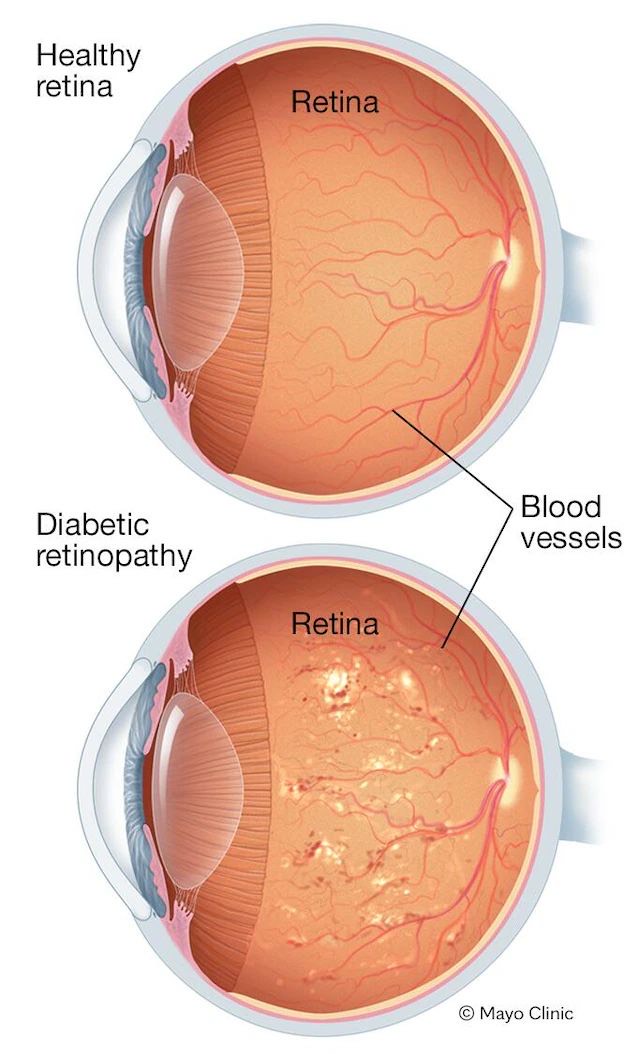
Diabetic retinopathy is a vision complication caused by diabetes. It’s caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina).
At first, diabetic retinopathy might cause no symptoms or only mild vision problems. But it can lead to blindness.
The condition can develop in anyone who has type 1 or type 2 diabetes. The longer you have diabetes and the less controlled your blood sugar is, the more likely you are to develop this eye complication.
Symptoms
You might not have symptoms in the early stages of diabetic retinopathy. As the condition progresses, you might develop the following symptoms:
- Spots or dark strings floating in your vision (floaters)
- Blurred vision
- Fluctuating vision
- Dark or empty areas in your vision
- Vision loss
When to see an eye doctor
Careful management of your diabetes is the best way to prevent vision loss. If you have diabetes, see your eye doctor for a yearly eye exam with dilation — even if your vision seems fine.
Developing diabetes when pregnant (gestational diabetes) or having diabetes before becoming pregnant can increase your risk of diabetic retinopathy. If you’re pregnant, your eye doctor might recommend additional eye exams throughout your pregnancy.
Contact your eye doctor right away if your vision changes suddenly or becomes blurry, spotty or hazy.
Causes
Over time, too much sugar in your blood can lead to the blockage of the tiny blood vessels that nourish the retina, cutting off its blood supply. As a result, the eye attempts to grow new blood vessels. But these new blood vessels don’t develop properly and can leak easily.
In the early stages of diabetic retinopathy, the walls of the blood vessels in your retina weaken. Tiny bulges protrude from the vessel walls, sometimes leaking or oozing fluid and blood into the retina. Tissues in the retina may swell, producing white spots in the retina. As diabetic retinopathy progresses, new blood vessels may grow and threaten your vision.
Risk factors
Anyone who has diabetes can develop diabetic retinopathy. The risk of developing the eye condition can increase as a result of:
- Having diabetes for a long time
- Poor control of your blood sugar level
- High blood pressure
- High cholesterol
- Pregnancy
- Tobacco use
Prevention
You can’t always prevent diabetic retinopathy. However, regular eye exams, good control of your blood sugar and blood pressure, and early intervention for vision problems can help prevent severe vision loss.
If you have diabetes, reduce your risk of getting diabetic retinopathy by doing the following:
- Manage your diabetes. Make healthy eating and physical activity part of your daily routine. Try to get at least 150 minutes of moderate aerobic activity, such as walking each week. Take oral diabetes medications or insulin as directed.
- Monitor your blood sugar level. You might need to check and record your blood sugar level several times a day — or more frequently if you’re ill or under stress. Ask your doctor how often you need to test your blood sugar.
- Ask your doctor about a glycosylated hemoglobin test. The glycosylated hemoglobin test, or hemoglobin A1C test, reflects your average blood sugar level for the two- to three-month period before the test. For most people with diabetes, the A1C goal is to be under 7%.
- Keep your blood pressure and cholesterol under control. Eating healthy foods, exercising regularly and losing excess weight can help. Sometimes medication is needed, too.
- If you smoke or use other types of tobacco, ask your doctor to help you quit. Smoking increases your risk of various diabetes complications, including diabetic retinopathy.
- Pay attention to vision changes. Contact your eye doctor right away if your vision suddenly changes or becomes blurry, spotty or hazy.
Remember, diabetes doesn’t necessarily lead to vision loss. Taking an active role in diabetes management can go a long way toward preventing complications.
